- The first cases of Aids were recorded four decades ago this year.
- So many years later, “the fight is far from over”. In 2020, nearly 700 000 people died from Aids-related complications.
- Although this figure marks a thirty-year low in deaths, each one was preventable.
Resource details:
Presentation title: HIV prevention 2021 – Where are we now and where are we going?
Speakers: Anthony Fauci (National Institute of Allergy and Infectious Diseases), Winnie Byanyima (The Joint United Nations Programme on HIV and AIDS)
Publication date: 27 January 2021
What the plenary is about:
In this opening session for the fourth HIV Research for Prevention (HIVR4P) conference, the speakers set the stage and provide an overview of some of the highlights in HIV prevention along with recent breakthroughs in the field. In the past 40 years, scientists and activists have grappled with many challenges around combatting the HIV pandemic — from combating HIV denialism to finding a vaccine for a complex virus. While the recent emergence of the new COVID-19 pandemic brings with it new challenges for HIV prevention, it also creates an opportunity to share knowledge and collaborate on fighting both outbreaks together.
Key take-aways from the speakers:
The pandemic pathway paved by HIV, as outlined by the US infectious disease expert, Anthony Fauci.
Lessons on the role of community
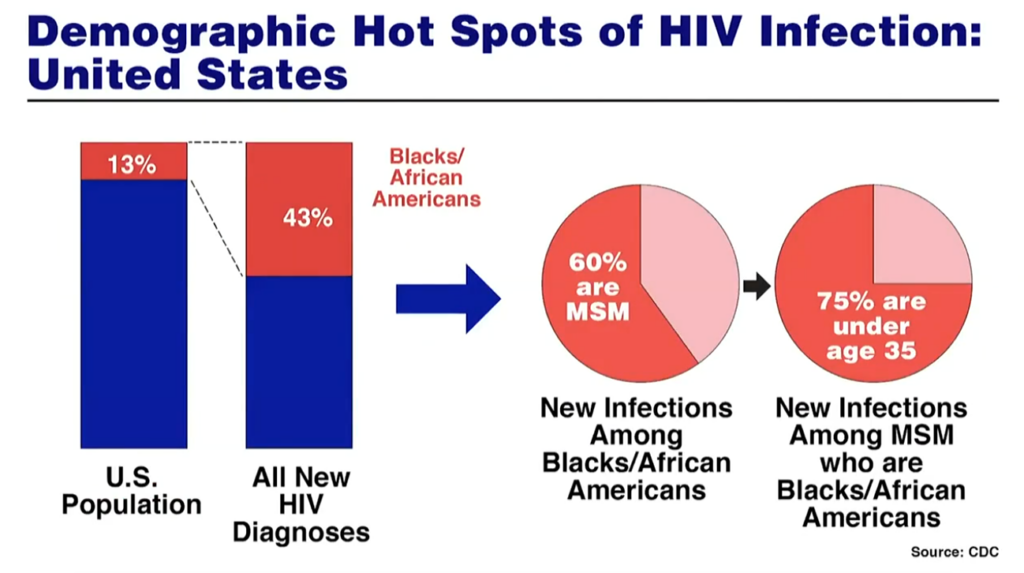
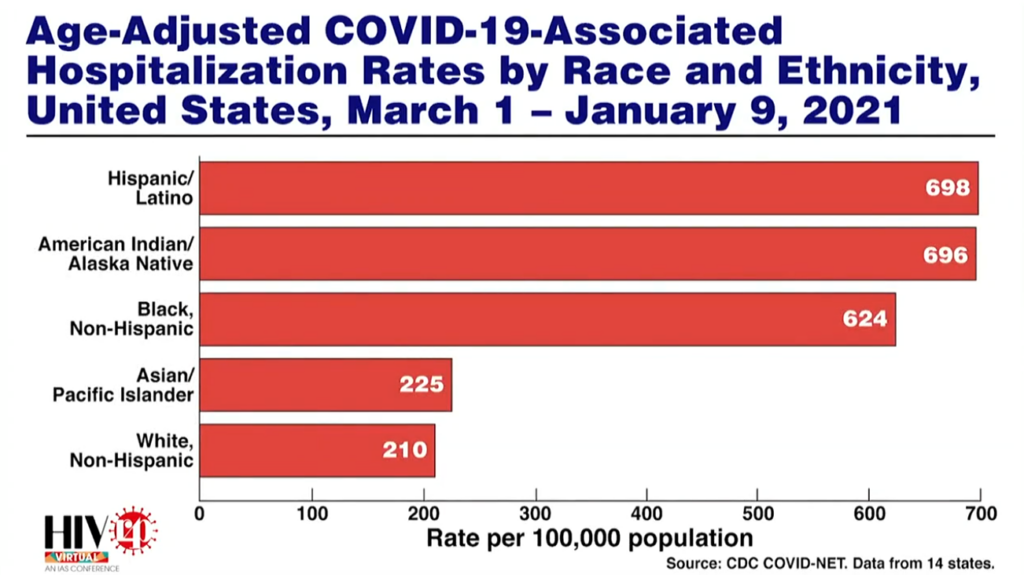
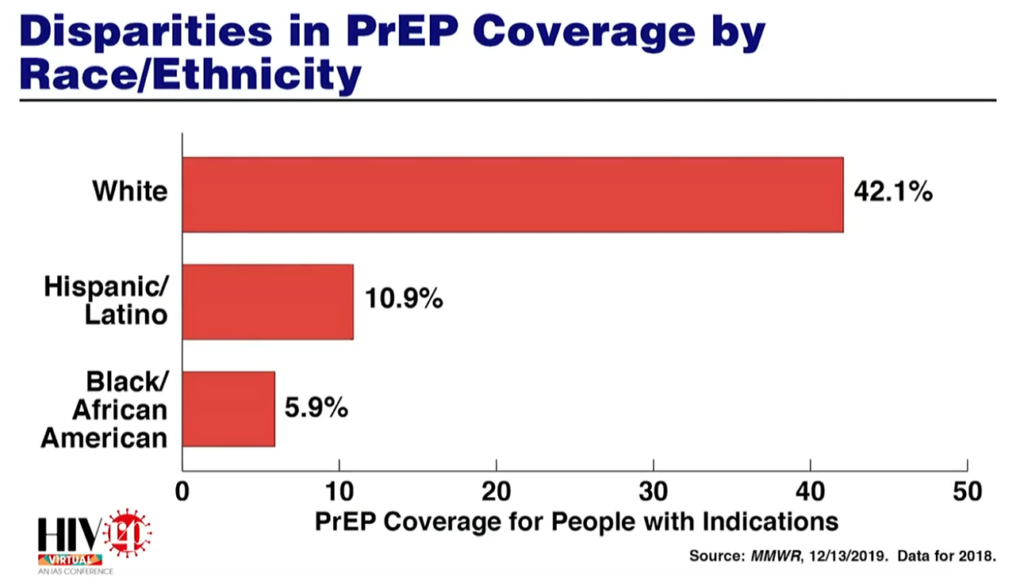
- As was seen with the HIV epidemic, there is once again a disproportionate burden of disease among communities of colour.
- 43% of new HIV infections are among African Americans in the United States, even though these communities only constitute 13% of the country’s overall population.
- This disparity of infections is also being reflected in the current COVID-19 pandemic.
- One of the lessons learned during the early stages of the HIV epidemic was the importance of researchers engaging with communities that are disproportionately affected by a disease.
- COVID-19 has been able to draw on the community engagement paradigm that was established for HIV.
- For example, the COVID-19 Prevention Network (CoVPN) is directly modelled on trial networks that were created for HIV and draws on years of expertise from people who have been running clinical trials for HIV vaccines.
- The accelerated timeline for COVID research has also relied on adapting these community engagement platforms. Fauci explains how his team has used their experience engaging with men who have sex with men on HIV prevention to reach out to native American populations on the need for vaccination.
- Fauci also emphasised the importance of “getting brown and black people vaccinating because of the understandable reluctance and hesitancy that they would have given the history of the relationship between federal funding, research projects and black and brown communities”.
Prevention in the absence of a vaccine
- “We don’t yet have a vaccine that is safe and effective for HIV,” says Fauci. “While that science continues, therapeutic interventions have played a critical role in HIV prevention.”
- The long and complicated journey to finding an HIV vaccine has led to major breakthroughs and success in non-vaccine prevention.
- This includes both treatment as prevention and the use of pre-exposure prophylaxis (PrEP), which is 99% effective at protecting people from infection — and work in this field is only continuing to get better. For example, the recent announcement of the use of long-acting cabotegravir.
- There is also work being done testing new ideas like whether antibodies from someone who has recovered from a disease or lab-made ones that mimic what your body naturally produces can be used to protect people from a virus. New evidence on the promising findings from the AMP trials, which tested this idea, was presented at the conference.
- Fauci says, “we borrowed from this strategy” and there are a number of studies testing this same approach of passive immunisation with antibodies underway for COVID-19.
The quest for a vaccine
- The race to find a vaccine for COVID-19 best exemplifies the synergy in research between the two pandemics.
- Fauci explains: “HIV vaccine development remains a challenge. However, advances in HIV vaccinology — even though we don’t yet have an HIV vaccine — has paved the way for SARS-CoV-2 vaccines.”
- Part of this is also because the nature of the COVID-19 pandemic has brought people from different fields together and allowed them to combine their research to find solutions to this new challenge.
- At the National Institute of Allergy and Infectious Diseases, Fauci says that years of work understanding the structure of HIV and how it links to vaccine development was used to help design jabs for various other virus outbreaks like MERS and now SARS-CoV-2.
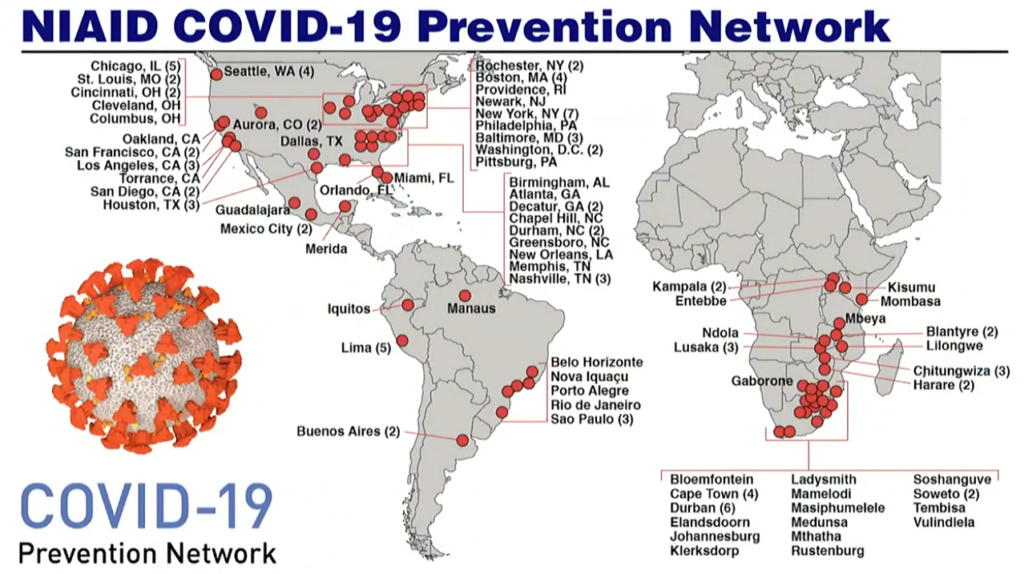
- This level of collaboration is also carrying over to clinical trials under the CoVPN consortium. Fauci explains: “Something that started as an idea years ago to build a domestic and international network of clinical trials that we never in our wildest dreams thought it would be used to counter and develop a vaccine for one of the most extraordinary pandemics.”
- The ability to go from sequencing a virus to having effective vaccines being rolled out in several countries in the span of 11 months is as a result of this expertise and years of work on other epidemics, says Fauci.
Denialism = murder
- The HIV outbreak saw tension between scientists and government officials, as some politicians continued to deny the reality of the virus. Fauci recalls at one point an outburst on denialism where he said: “This is murder. It’s really just that simple.”
- For Fauci, the continuous denial of the epidemic has become overwhelming. “To deny the reality of an epidemic that we were experiencing was really nothing short of causing the deaths of people.”
- Now, almost 14 years later, he says the world is once again experiencing the same kind of denialism when it comes to COVID-19. With people referring to a virus that killed millions of people globally “as a hoax or something that doesn’t exist”.
- This challenge of denialism and people not confronting the tragic consequences of these pandemics is “a challenge that we will continue to be facing,” he says.
How far will the fight against HIV be in 2025?
The fight is far from over
- 2021 marks 40 years since the first reported cases of Aids. But so many years later, “the fight is far from over”, says Winnie Byanyima, the executive director of The Joint United Nations Programme on HIV and Aids, UNAids.
- There were still 1.7-million new HIV infections recorded in 2020, and 690 000 Aids-related deaths.
- New infections were the lowest they’ve been since 1988 and the reduction in deaths is “historic” but Byanyima warns against becoming complacent.
- Why? Because every Aids-related death is preventable. “The truth is we are failing. We have missed our targets for 2020 by a wide margin – we need a wakeup call.”
- While the COVID-19 pandemic brought to light the fragility of the global HIV response as the pandemic interrupted care for millions around the world, the outbreak also showed how quickly solutions can come about when there is a shared sense of urgency, Byanyima argues.
Inequality drives a widening gap in access to HIV prevention tools
- Research presented at the International Aids Society’s HIV Research for Prevention conference showed remarkable new technology is on the way to help people protect themselves against HIV.
- For example, a two-monthly injection may soon be on the horizon. Long-acting cabotegravir was shown to be 89% more effective than the oral pre-exposure prophylaxis pill, called Truvada. Read more about this advancement and others here.
- But, warns Byanyima: “Prevention technology means little if people can’t access it and to those who don’t feel prevention works for them.”
- Promising results from clinical trials must be made applicable to people at a community level, Fauci says.
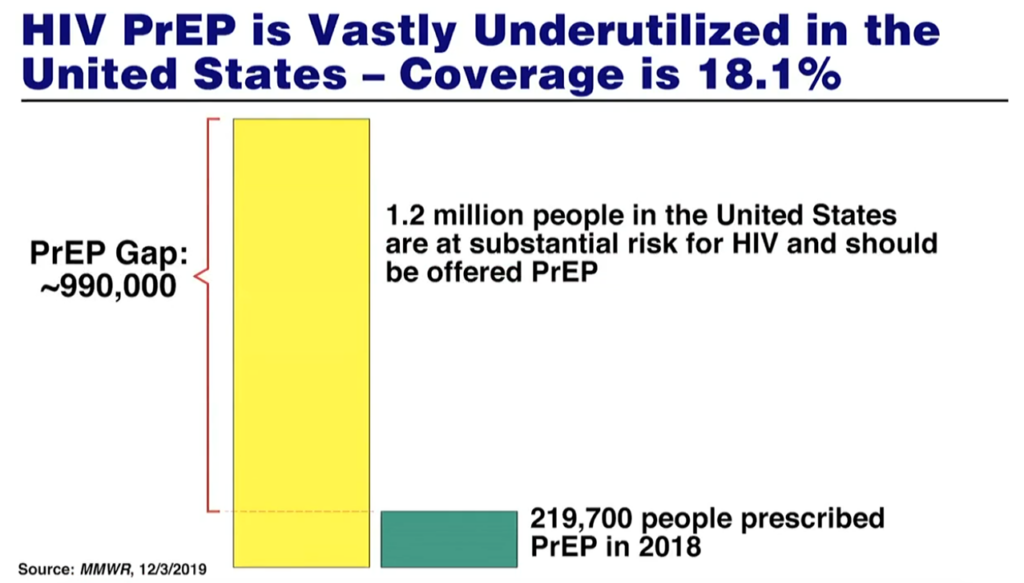
- In the United States for example, there are 1.2-million people at risk of contracting HIV yet only about 200 000 people were prescribed PrEP in 2018. In this case, Fauci explains, the successful results of clinical trials showing PrEP works well to protect people didn’t translate into the real world because it wasn’t implemented into the health system well.
- Between 2010 and 2019 overall HIV infections fell, but increased for some groups (such as sex workers, transgender women, people who inject drugs and gay men).
- “The difference is access [to HIV prevention services],” explains Byanyima.
How to get PrEP to the people
- Serious effort must go into the decriminalisation of sex work. Research has shown this policy could slow the epidemic. Read more here.
- People who are the most at risk of HIV infection, such as sex workers and transgender women, must be the first to receive HIV prevention medication.
- In 2019, adolescent girls and young women in Sub-Saharan Africa made up 25% of all new HIV infections. Countries must prioritise easy access to the newest prevention tools for young women and girls and remove policies that say only some people can get them.
- Global UNAids targets aim to get HIV prevention tools to 95% of people at high risk of HIV infection “We will never end Aids if we don’t make prevention a priority,” Byanyima says.
Is there any good news?
- For the first time, UNAids’ HIV targets also include goals to create “supportive policy environments” that makes it easy for people to access the care they need.
- UNAids estimates that if HIV prevention targets are met, 2.6-million new HIV infections and 440 000 Aids-related deaths can be prevented.








